Viewing archives for Bladder, Bowel, Sexual Function
ImPRESS: Improving Pelvic Rehabilitation using Epidural Stimulation after SCI
What you need to know
Institution:
Royal National Orthopaedic Hospital
Lead researcher:
Dr. David Baxter
Functional target:
Bowel, bladder, sexual function
Treatment type:
Neuromodulation, Rehabilitation
- While the bladder and bowel are relatively simple organs, their control system is highly complex and becomes severely compromised following a Spinal Cord Injury (SCI).
- Existing bowel management techniques are far from ideal as around half of people living with SCI continue to experience incontinence, constipation and infections.
- Improving bowel management is a major priority among people living with a SCI.
In a nutshell
Recently, studies exploring epidural stimulation (stimulation of the spinal cord) for restoration of motor function after SCI have identified important improvements in pelvic (bladder and bowel) functions. In this trial we will explore epidural stimulation specifically targeting bowel function in people with SCI.
This study will recruit volunteers with SCI to undergo a short trial with epidural stimulation.This will involve the surgical implantation of electrodes close to the spinal cord, in the epidural space, whilst the device and wires are placed external to the body. Stimulation will initially be trialled in hospital to measure the effects on bladder and bowel function; then volunteers will trial stimulation at home alongside their usual bladder and bowel management.
People who respond well to the trial will then be offered a fully implantable epidural stimulator. We will ask them to use their stimulator at home for 8 weeks whilst performing a programme of pelvic floor muscle training. Before and after the programme, we will measure their bowel function. At the end of the trial, volunteers can have their implanted devices removed or keep them.
How this supports our goal to cure paralysis.
Restoration of bowel, bladder and sexual function are rated among the highest priorities for recovery in individuals with SCI. Not only do these conditions individually impact the health-related quality of life, but they also have life-threatening complications. For example, stimuli from bladder (during care, catheterization, or evaluation) are the most frequent triggers of severe episodes of hypertensive crisis known as autonomic dysreflexia. Despite this, the vast majority of research is focused on overt disabilities following SCI (e.g., motor paralysis), whereas more devastating ‘invisible’ disabilities, like pelvic organ dysfunctions, are unfortunately understudied.
This research could help develop a safe and long-term route to improving these critical functions for those living with paralysis. This would be life changing, helping to restore freedom, and dignity to the community.
You may also be interested in
Promoting Restoration of Function of Co-ordinated Bladder Storage and Voiding following SCI
What you need to know
Institution:
London Spinal Cord Injury Centre
Lead researcher:
Dr. Sarah Knight
Functional target:
Bowel, bladder, sexual function
Treatment type:
Neuromodulation, Rehabilitation
- Normal bladder function includes a storage phase and a voiding phase, these processes work in a coordinated manner allowing for controlled maintenance of continence, until a socially convenient time.
- After a spinal cord injury, this control is lost, resulting in a profound impact on an individual’s quality of life as well as their physical health due to recurrent urinary tract infections and potential kidney damage.
- Researchers aim to combine transcutaneous spinal cord stimulation (tSCS) with a bladder training programme with a view to restore bladder function.
In a nutshell
Many pelvic functions including the bladder, bowel and sexual organs are controlled by a complex set of neurophysiological interactions which include lumbo-sacral reflexes of the spine. Following a spinal cord injury the pathways associated with these reflexes are disrupted, resulting in a loss of coordinated bladder, bowel, and sexual function.
In an attempt to restore bladder function, researchers will work with twenty individuals who sustained a complete or incomplete spinal cord injury in the past six months. These individuals will be assessed at baseline using a series of questionnaires which examine their symptoms and various aspects of their quality of life.
These individuals will receive transcutaneous spinal cord stimulation which involves the application of electrodes on the skin, positioned over the thoraco-lumbar spinal cord.
Researchers will then work with a group of participants to deliver specialised bladder reflex training techniques. The study will look to see the difference between these participants and a control group who would continue with their usual bladder management routine.
The expectation is that using a combined approach (stimulation plus specialist training) will result in increased bladder capacity and ultimately support voluntary bladder emptying.
How this supports our goal to cure paralysis.
By offering this potential improvement in bladder function, tSCS not only reduces the physical discomfort and inconvenience caused by bladder issues but also contributes significantly to an individual’s sense of independence and overall quality of life.
Transcutaneous spinal cord stimulation is a non-invasive technique which offers hope for enhancing bladder function in individuals with spinal cord injuries The stimulation delivered through tSCS can support communication between the spinal cord and the bladder, potentially restoring some spinal cord injuries (SCIs). This reduces the risks associated with invasive procedures and minimizes patient burden, empowering individuals to manage their condition outside clinical settings.
You may also be interested in
Non-invasive neuromodulation to treat bladder, bowel and sexual dysfunction following spinal cord injury
What you need to know
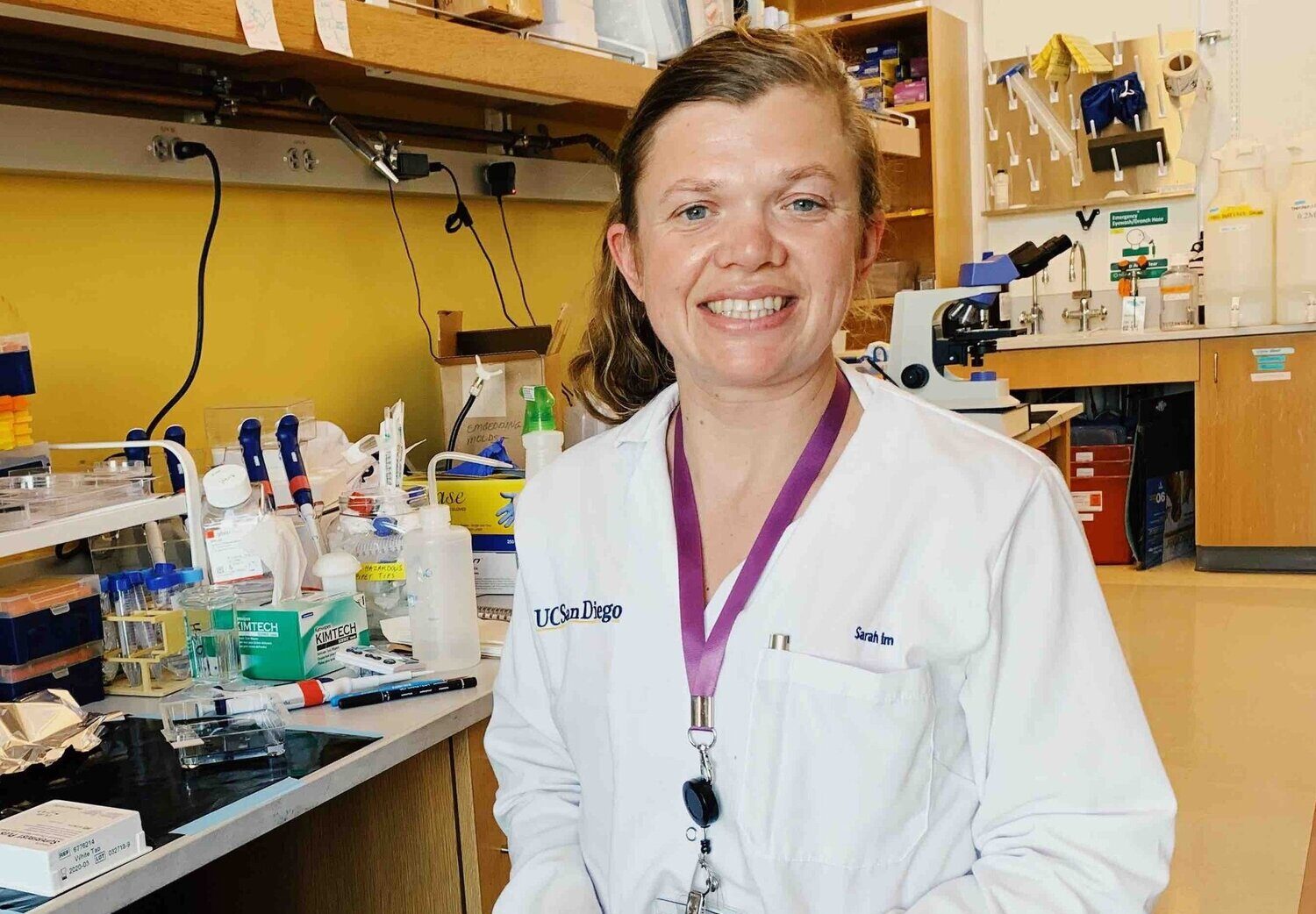
Lead researcher:
Prof. Andrei Krassioukov
Functional target:
Bowel, bladder, sexual function
Treatment type:
Neuromodulation, Rehabilitation
- Research shows that autonomic recovery (i.e. bladder, bowel and sexual function) is a priority for people living with spinal cord injury (SCI). However there is still a major lack of research dedicated to improving this for people living with spinal cord injury (SCI).
- This clinical study examines the effects of “transcutaneous” (over the skin) electrical stimulation of the spinal cord (TCSCS) on promoting recovery of bladder, bowel and sexual functions in individuals with SCI.
- This non-invasive therapeutic method involves the application of electrodes over the skin, and is based on ground-breaking work which has shown that spinal cord stimulation can promote functional recovery in individuals with chronic (long-term) SCI.
In a nutshell
- Establish stimulation parameters (i.e., electrode positioning/stimulation intensity) necessary for TCSCS to activate the bladder, bowel and skeletal muscles responsible for successfully passing urine & faeces.
- Monitor the long-term (6 weeks) beneficial effects of TCSCS on bladder, bowel, and sexual functions.
To assess the potential for TCSCS to offer a simple, cost-effective solution to treat autonomic dysfunctions (i.e., urine and faecal incontinence, erectile and vaginal lubrication difficulties etc.) that would significantly improve overall health-related quality of life for individuals with SCI.
How this supports our goal to cure paralysis.
Restoration of bowel, bladder and sexual function are rated among the highest priorities for recovery in individuals with SCI. Not only do these conditions individually impact the health-related quality of life, but they also have life-threatening complications. For example, stimuli from bladder (during care, catheterization, or evaluation) are the most frequent triggers of severe episodes of hypertensive crisis known as autonomic dysreflexia.
Despite this, the vast majority of research is focused on overt disabilities following SCI (e.g., motor paralysis), whereas more devastating ‘invisible’ disabilities, like pelvic organ dysfunctions, are unfortunately understudied.
Transcutaneous spinal cord stimulation could offer a simpler and cost-effective solution that utilizes readily available, inexpensive, conventional electrodes with an established safety profile. Findings from this study may ultimately lead to the development and commercialization of new treatments strategies resulting in a reduced burden of care and improved quality of life for people with chronic SCI.
You may also be interested in
Development of epidural electrical stimulation for bladder control: animal model
What you need to know
Institution:
Leeds University
Lead researcher:
Dr. Ronaldo Ichiyama
Functional target:
Bowel, bladder, sexual function
Treatment type:
Neuromodulation
- Epidural electrical stimulation (EES) describes a technique whereby an electrode is implanted into in the epidural space. This electrode can transmit electrical currents to cause targeted muscle contractions.
- Researchers are using animal models to investigate the effectiveness of EES on the recovery of bladder function in the post-acute and chronic stages of spinal cord injury.
- Preliminary studies have shown that EES paired with bladder rehabilitation is associated with the recovery of certain biological markers associated with bladder function.
In a nutshell
The coordination of bladder muscles is complex. When they get disrupted after spinal cord injury, messages are no longer able to pass between the bladder and brain. Resulting complications include high bladder pressure, incontinence, incomplete emptying and reflux, along with recurrent bladder infections, stones, kidney distension and inflammation and even renal failure. Although current treatments can provide some recovery of function, none are able to fully restore function to its pre-injury condition.
Researchers have conducted a series of studies to better understand the physiological processes underlying bladder function that are affected by post spinal cord injury.
Measuring bladder function in animals is a challenging undertaking. To achieve this, researchers have worked on developing a first-of-its-kind catheter which can be used to measure specific physiological markers, these are (1) bladder pressure and (2) external urethral sphincter contraction.
This has laid the groundwork for further studies which have used mice to investigate the effects of epidural electrical stimulation, combined with a rehabilitation protocol. Early studies have demonstrated an improvement in bladder function in mice 48 hours after injury. Follow-up studies will work on fine tuning bladder training protocols and EES parameters and with a focus on how this procedure can benefit patients with a chronic spinal cord injury.
How this supports our goal to cure paralysis.
Recovery of bladder function has been widely considered one of the top priorities among individuals with SCI. The clinical benefits, and enhancement in quality of life that recovery of such autonomic functions can provide are multifaceted and far reaching. Such recovery could alleviate secondary issues related to bladder management, e.g. urinary infections and autonomic dysreflexia.
With the current advancements in EES implants, researchers are hopeful about swiftly applying this intervention in clinical settings. Collaborative efforts in partnership with major spinal centers are underway with the aim of trialing EES for individuals with SCI. While initial research has primarily concentrated on enhancing locomotion and bowel function, the focus is now expanding to include bladder function.
You may also be interested in
Novel regenerative therapies for restoring sensory function after spinal cord injury
What you need to know
Institution:
King's College London
Lead researcher:
Prof. Elizabeth Bradbury
Functional target:
Bowel, bladder, sexual function
Treatment type:
Pharmacological
- Spinal cord injuries often result in damage to sensory nerve fibers that carry signals from the body to the brain, this can result in impaired bladder, bowel, and sexual function. Researchers are now investigating how damaged sensory nerve fibers can be repaired.
- Studies conducted using animal models, have identified three molecules that are associated with neural regeneration (α9 integrin, kindlin-1 and chondroitinase), specifically for the benefit of upper limb function.
- Researchers now hope to deliver these molecules to additional nerves in the hopes of restoring bladder function. To do this, researchers will investigate the most effective methods for delivering these molecules at a biochemical level. They will then determine which nerves are best suited to receiving these injections.
In a nutshell
Sensory fibers are specialized nerve fibers responsible for transmitting sensory information from the body to the brain. This allows us to recognize certain sensations such as: the need for a bowel movement, bladder fullness, or sexual arousal. Damage to sensory fibers following spinal cord injury can affect various bodily functions, including those related to the bladder, bowel, and sexual activities.
Previous studies using animal models have demonstrated that injecting certain molecules can promote the regeneration of sensory fibers and improve sensory function in the upper limbs. Three molecules have been identified, the first two called α9 integrin and kindlin-1 have been shown to trigger a growth response in the fibers, whilst the third molecule called chondroitinase has shown that it can overcome scar tissue. Researchers will build on these findings to better understand how these same molecules can be delivered to other sensory nerves, responsible for bladder function.
How this supports our goal to cure paralysis.
The wall of the bladder is made up of a collection of muscle fibers which are known as the detrusor muscle. Muscle fibers are woven together in a way that allows the bladder to stretch and contract in response to the presence of urine.
To coordinate this activity, nerves send messages via the spinal cord to various muscles, including the detrusor muscle in the bladder. In individuals with spinal cord injury, these signals are disrupted due to damaged nerve fibers. Researchers hope that their work can allow for the regeneration of these nerve fibers to restore bladder function, ultimately allowing individuals to regain their dignity and independence.
You may also be interested in